Introduction
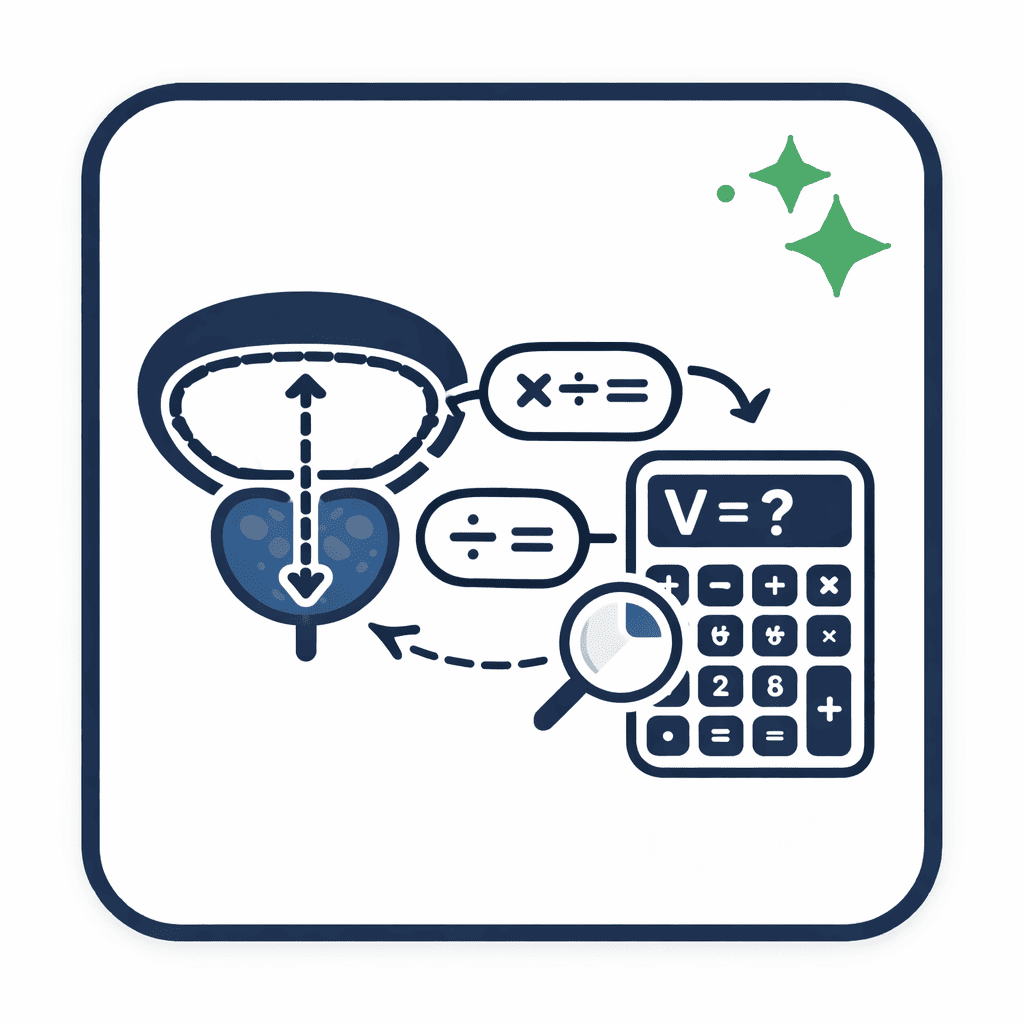
Prostate volume calculation underpins clinical decision-making in benign prostatic hyperplasia (BPH) management, prostate-specific antigen (PSA) density assessment and treatment planning for prostate cancer. Digital and manual tools known collectively as the prostate volume calculator translate sonographic or magnetic resonance imaging (MRI) dimensions into volumetric measurements. Precision in these calculations influences therapeutic choices—such as initiation of 5α-reductase inhibitors or selection of surgical approaches—and informs risk stratification. This analysis examines how prostate volume calculators work, the prostate volume formula, comparative prostate volume measurement methods, validation of prostate volume calculator accuracy, and considerations for interpret prostate volume in routine practice.
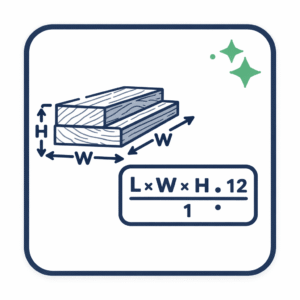
Mathematical Basis: Prostate Volume Formula
Prostatic volume is usually modeled as an ellipsoid. The standard prostate volume formula derives from the ellipsoid equation:
Volume (cc) = Length × Height × Width × 0.523 [Radiology Tutor]
Where:
- Length (L) is the craniocaudal (longitudinal) measurement in centimeters.
- Height (H) is the anteroposterior (AP) diameter in centimeters.
- Width (W) is the maximum transverse diameter in centimeters.
- 0.523 approximates π/6, the constant for converting rectangular dimensions into an ellipsoid volume.
An alternative expression uses π/6 explicitly:
Volume (cc) = (L × H × W) × (π/6)
Imaging Methods for Prostate Volume Measurement
Transrectal Ultrasound (TRUS)
TRUS remains the most common modality. A bi-planar transducer acquires longitudinal, anteroposterior and transverse diameters. The ellipsoid assumption provides rapid estimation. A validation study of 153 prostatectomy specimens found that ellipsoid calculation with coefficient 0.52 underestimated true volume by 10–20 percent, prompting some centers to adopt an adjusted coefficient of 0.66 to improve accuracy. [J Urol. 1992;148(6):1736–40]
Transabdominal Ultrasound (TAUS)
TAUS offers non-invasive volumetry via suprapubic scanning. A machine learning–augmented TAUS model achieved mean absolute errors under 7 cc compared to TRUS, with minimal operator experience required. [Natali et al. 2020]
Magnetic Resonance Imaging (MRI)
MRI enables multiplanar volumetry. Planimetric segmentation—tracing gland contours slice by slice—yields the highest fidelity, while the ellipsoid method correlates strongly with segmented volumes (R ≈ 0.99). [PI-RADS v2.1 update]
Prostate Volume Calculator Tools
Ultrasound Console Integration
Vendors such as Philips and Siemens embed volumetry modules within TRUS systems. After inputting L, H and W, the console applies the prostate volume formula automatically and displays volume in cubic centimeters.
Web-Based Calculators
Online tools prompt dimension entry via forms and compute volumes instantly. No installation is required, facilitating peer review of measurements and patient discussions. [Radiology Tutor]
Mobile Applications
Smartphone apps allow clinicians to input ultrasound-derived measurements at point of care. Accuracy depends on precise data entry and consistent unit notation; small probe angulation changes may introduce 5–10 percent volume error.
Automated AI-Driven Systems
Deep-learning frameworks analyze ultrasound or MRI images to segment the prostate and calculate volume without manual calipers, yielding estimates within 5 percent of manual ellipsoid methods. [Albayrak et al. 2020]
Sources of Variability
- Probe Angulation: 5–10° deviations can alter diameter measurements by 2–3 mm, leading to volume variation up to 15 percent.
- Coefficient Selection: Use of 0.52 versus locally derived constants (0.60–0.66) shifts absolute volumes.
- Inter-Observer Differences: Standardized training reduces measurement variance from 10–12 percent to under 5 percent.
- Image Quality: Shadowing, calcifications or patient motion may obscure gland boundaries and complicate caliper placement.
Validation and Reliability
- TRUS vs. Pathology: Correlation coefficients (r) of 0.89–0.94 with systematic underestimation of 10–20 percent. [J Urol. 1992;148(6):1736–40]
- Ellipsoid vs. Planimetry on MRI: ICC of 0.992 and ellipsoid bias under 5 percent for volumes up to 80 cc. [PI-RADS v2.1 update]
- TAUS vs. TRUS Machine Learning: Mean absolute error of 6.8 cc. [Natali et al. 2020]
Clinical Applications
Volume measurements guide therapy in BPH:
- < 30 cc: α-blocker monotherapy
- 30–80 cc: Combination α-blocker and 5α-reductase inhibitor [AUA BPH Guideline]
- > 80 cc: Surgical intervention (e.g., laser enucleation)
PSA density (PSAD) integrates gland size:
PSAD = Serum PSA (ng/ml) ÷ Prostate Volume (cc) [Wikipedia]
Emerging Technologies
AI-driven segmentation promises automated volumetry with minimal user input, reducing operator time by 80 percent while maintaining accuracy within 5 percent of manual methods. Integration into PACS/EHR systems supports longitudinal tracking of prostate growth and treatment response.
Final Considerations
Prostate volume calculators operationalize the ellipsoid-based prostate volume formula to convert imaging measurements into quantitative gland volumes. Mastery of how prostate volume calculators work, awareness of imaging modalities and adherence to standardized measurement protocols enhance calculate prostate volume reliability. As AI-driven and integrated reporting tools evolve, clinicians will benefit from improved workflow efficiency and data-driven insights into prostate health.