Prostate Volume Calculator
Estimate prostate volume using the ellipsoid formula:
Volume ≈ Length × Width × Height × 0.523
Results
| Volume | — mL (≈ cc) |
|---|---|
| Volume | — in³ |
Note: 1 mL ≈ 1 cm³. This calculator is for educational/estimation use.
Introduction
Prostate volume calculation underpins clinical decision-making in benign prostatic hyperplasia (BPH) management, prostate-specific antigen (PSA) density assessment and treatment planning for prostate cancer. Digital and manual tools known collectively as the prostate volume calculator translate sonographic or magnetic resonance imaging (MRI) dimensions into volumetric measurements. Precision in these calculations influences therapeutic choices—such as initiation of 5α-reductase inhibitors or selection of surgical approaches—and informs risk stratification. This analysis examines how prostate volume calculator works, the prostate volume formula, comparative prostate volume measurement methods, validation of prostate volume calculator accuracy, and considerations for interpret prostate volume in routine practice.
Mathematical Basis: Prostate Volume Formula
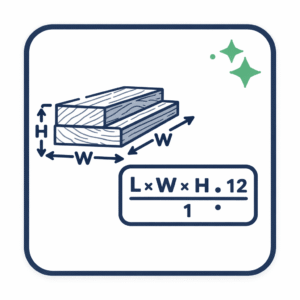
Prostatic volume is usually modeled as an ellipsoid. The standard prostate volume formula derives from the ellipsoid equation:
Volume (cc) = Length × Height × Width × 0.523 [Radiology Tutor]
Where:
- Length (L) is the craniocaudal (longitudinal) measurement in centimeters.
- Height (H) is the anteroposterior (AP) diameter in centimeters.
- Width (W) is the maximum transverse diameter in centimeters.
- 0.523 approximates π/6, the constant for converting rectangular dimensions into an ellipsoid volume.
An alternative expression uses π/6 explicitly:
Volume (cc) = (L × H × W) × (π/6)
Imaging Methods for Prostate Volume Measurement
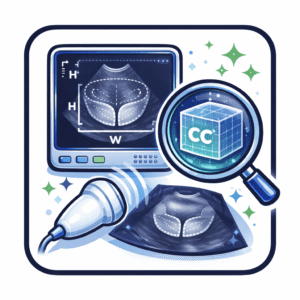
Transrectal Ultrasound (TRUS)
TRUS remains the most common modality. Operators obtain three orthogonal dimensions—longitudinal, AP and transverse—via a transrectal probe. The ellipsoid assumption provides rapid estimation. In a series of fresh prostatectomy specimens, standard ellipsoid calculation (coefficient 0.52) underestimated true volume by approximately 13 percent, prompting some institutions to adjust the coefficient to 0.66 to improve accuracy.
Transabdominal Ultrasound (TAUS)
TAUS offers non-invasive volumetry, particularly in primary-care settings. Dimensions are acquired via suprapubic scanning. Accuracy is slightly lower than TRUS; a machine-learning–augmented TAUS model achieved mean absolute errors under 7 cc compared to TRUS benchmarks, with minimal operator experience required.
Magnetic Resonance Imaging (MRI)
MRI provides high-resolution, multiplanar images. Volumetry may use manual planimetry—tracing cross-sectional areas on each slice—or the ellipsoid formula. Planimetric segmentation yields the highest fidelity but is time-intensive; ellipsoid calculation on MRI correlates strongly with segmented volumes (R ≈ 0.99).
Prostate Volume Calculator Tools
Ultrasound Console Integration
Major vendors (e.g., Siemens, Philips) embed volumetry calculators within TRUS consoles. Upon measuring L, H and W, the system applies the ellipsoid formula automatically, displaying volume in cubic centimeters.
Web-Based Calculators
Online calculators such as Radiology Tutor’s prostate volume tool prompt entry of dimensions and compute volume instantly. These widgets require no installation and provide immediate feedback.
Mobile Applications
Smartphone apps allow clinicians to input ultrasound-derived dimensions at point of care. Their prostate volume calculator accuracy depends on correct data entry and consistent unit notation, with minor probe angulation changes translating to 5–10 percent volume error.
Automated AI-Driven Systems
Emerging deep-learning frameworks analyze 2D ultrasound or MRI images to segment the prostate automatically and calculate volume without manual measurement, yielding estimates within 5 percent of manual ellipsoid calculations.
Accuracy and Reliability
- TRUS vs. Pathology: Correlation coefficients between TRUS ellipsoid volumes and prostatectomy specimens range from 0.89 to 0.94, with systematic underestimation of 10–20 percent.
- Ellipsoid vs. Planimetry: Ellipsoid calculation on MRI correlates with planimetric volumes at R ≈ 0.99.
- TAUS vs. TRUS: Machine-learning–augmented TAUS estimates differ from TRUS benchmarks by a mean absolute error of 6.8 cc.
Sources of variability include probe placement, coefficient selection and observer training; standardized protocols can reduce interobserver error below 5 percent.
Clinical Interpretation of Prostate Volume
Prostate size meaning extends beyond mere measurement: volume correlates loosely with lower urinary tract symptoms (LUTS) but strongly with risk of acute urinary retention and BPH progression. Treatment thresholds include:
- < 30 cc: α-blocker monotherapy
- 30–80 cc: Combination α-blocker and 5α-reductase inhibitor [AUA BPH Guideline]
- > 80 cc: Surgical intervention (e.g., laser enucleation)
PSA density (PSAD) normalizes PSA by gland volume (PSA Density):
PSAD = Serum PSA (ng/ml) ÷ Prostate Volume (cc)
Limitations and Future Directions
Ellipsoid assumptions inadequately capture irregular nodularity. Research into shape-adaptive coefficients and multiparametric segmentation seeks to refine methods. Fully automated AI systems promise throughput gains but require transparent validation and expert oversight for clinical adoption.
Integration within electronic health records enables longitudinal tracking of prostate size and PSA density, supporting population-level analytics and individualized patient management.
Final Considerations
Accurate prostate volume measurement methods—from TRUS and TAUS to MRI and AI-driven systems—rely on mastery of how prostate volume calculator works and the underlying prostate volume formula. Recognition of sources of variability, adoption of standardized protocols and periodic validation against reference standards enhance prostate size reliability. As technology evolves, seamless integration into clinical workflows will support precise, data-driven urological care.